AD This article contains links
Urinary incontinence is the inability to control your bladder, causing unwanted and involuntary leakage of urine1. The condition can affect anyone, at any age, but it is often a subject people avoid talking about. It is important you receive the correct diagnosis and treatment and talking to a healthcare professional is the first step.
There are different types of urinary incontinence, including;
- Stress incontinence: the involuntary loss of urine when your bladder is under pressure
- Urge incontinence: a sudden, intense urge to pass urine which cannot be suppressed
- Overflow incontinence: the inability to fully empty your bladder, causing frequent leaking
- Total incontinence: the inability of the bladder to store urine, causing constant passing of urine or frequent leaking
- Mixed incontinence: a mixture of both stress and urge urinary incontinence2
Treating Incontinence
Treatment for incontinence is very dependent on you as an individual and the type of incontinence you have. Sometimes more than one treatment is needed. Discussing the best treatment for you with your healthcare professional means you will receive the best help on how to manage and improve your incontinence symptoms. Treatments include;
- Pelvic floor exercises to strengthen the muscles surrounding the bladder3
- A change in your diet4
- Medication3
- Surgery may be a last resort if other treatments are not working3
Lifestyle Advice
Along with the above treatments, changes in your lifestyle can help manage incontinence. Normalising fluid intake, drinking between 1.5 and 2 litres on a daily basis, will reduce the risk of infection and bladder irritation4. Caffeinated drinks, alcohol and carbonated drinks should also be avoided, as these irritate the bladder4.
Additionally, caffeinated food such as dark and milk chocolate should be avoided, as well as acidic foods4. Once again, this lifestyle advice is all dependent on you as an individual and takes into consideration that there are no other contraindications.
Types Of Continence Products And How They Can Help You
In addition to lifestyle changes, continence products can help improve your quality of life. The product you use is your personal choice, although advice should be taken from your healthcare professional. Depending on the type of incontinence you have, a range of products are available including pads, external continence devices and catheters.
Different types of catheters exist, but catheters for intermittent self-catheterisation (ISC) are most often recommended5. A catheter is a tube which is placed into the bladder via the urethra (water pipe) which allows the urine to drain through an internal channel. ISC can be used if the individual is unable to empty their bladder fully which may be due to accidents resulting in spinal injuries or conditions such as multiple sclerosis, spina bifida, Parkinson’s disease or diabetes mellitus for example6.
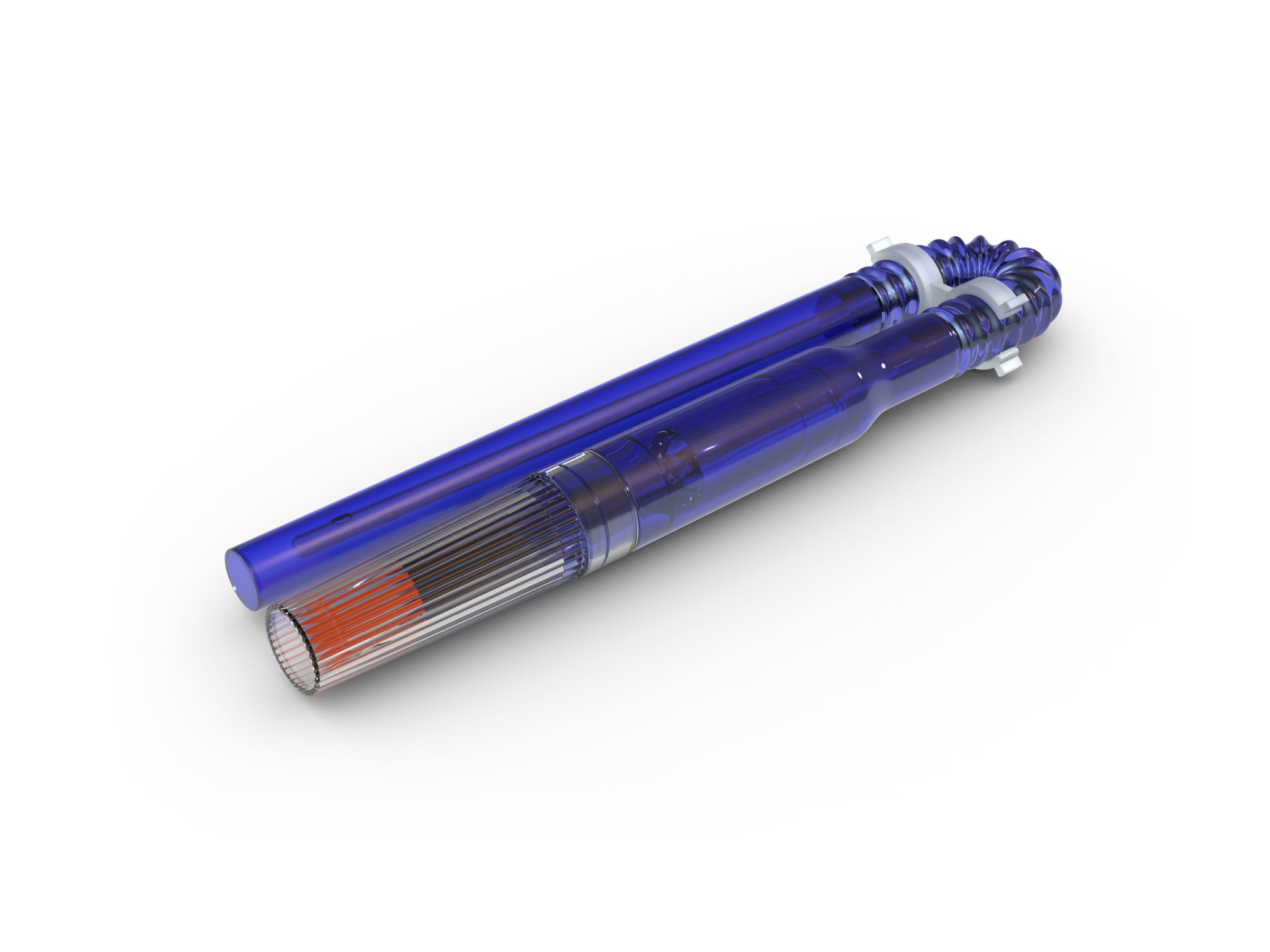
However, ISC might not be suitable for those with limited dexterity. Intermittent catheters are used on average 3-5 times a day to drain your bladder and then are removed, giving you freedom and independence. Lengths, sizes and coatings of intermittent catheters vary too. All Curan® catheters from CliniMed® are sterile and single-use. The compact Curan Man and Curan Lady catheters have a hydrogel coating and are mess-free with no liquid spillage. Alternatively, Curan Advantage intermittent catheters have a smooth hydrophilic ComfortCoat® with an integrated water sachet and are available in female, male and unisex lengths.



For men, urinary sheaths are another incontinence product option. Urinary sheaths are placed over the penis and allow the urine to drain away from the skin into a drainage bag. Alternatively, BioDerm®, an external continence device for men sticks only to the tip of the penis. Amongst other benefits, it is suitable for men experiencing leakage or sheaths falling off, or men who are sheath users and have broken skin. Both sheaths and BioDerm can be attached to a leg bag during the day or a night drainage bag through the night to collect the urine.


Incontinence pads are available for men and women. Pads draw urine away from the surface, keeping the skin dry and have the benefit of allowing those who may otherwise be housebound to get out and about7. An alternative to all these options would be an indwelling catheter, but this is often a last resort. Indwelling catheters are held in the bladder long-term by a balloon inflated with water and are connected to a urine collection bag. Indwelling catheters are usually replaced every 3 months, but this can vary if a person experiences catheter blockages or frequent infections.
About Us
At CliniMed we offer a range of urology and continence products to suit each patient’s needs. CliniMed’s mission involves developing healthcare products and services that enhance and improve lives, and this year alone we have launched two new ISC catheters into our range. To find out more about any of our continence products or to speak to one of our advisors about alternative products or services that could work for you, call us on the CliniMed Careline 0808 159 8020 or visit our website here.
References
- Royal College of Nursing. (2016) Continence. Introduction. Available at: https://rcni.com/hosted- content/rcn/continence/introduction (Accessed: 03/10/18)
- NHS. (2016) Urinary Incontinence. Overview. Available at: https://www.nhs.uk/conditions/urinary- incontinence/ (Accessed: 04/10/18)
- Age UK. (2018) Incontinence. Information and Advice. Available at: https://www.ageuk.org.uk/information-advice/health-wellbeing/conditions-illnesses/incontinence/ (Accessed: 02/10/18)
- Bladder Health UK. (2018) Continence Support. Treatments. Available at: http://bladderhealthuk.org/bladder-conditions/continence-support/treatments (Accessed: 03/10/18)
- NHS. (2017) Urinary Catheters. Types. Available at: https://www.nhs.uk/conditions/urinary-catheters/types/ (Accessed: 15/10/18)
- Spinks, J. (2013) Urinary incontinence and the importance of catheter fixation. JCN. Vol 27, No5.
- NHS. (2016) Urinary Incontinence. Incontinence Products. Available at: https://www.nhs.uk/conditions/urinary-incontinence/incontinence-products/ (Accessed: 15/10/18)
PID 6673









