What Is A Fistula And What Causes Them?
Fistulas are usually caused by injury or surgery, they may also form after an infection has led to severe inflammation. Inflammatory bowel conditions such as Crohn’s Disease and Ulcerative Colitis are examples of conditions that lead to fistulas forming, for example, between two loops of intestine. There are many different types of fistula such as an anal fistula or rectovaginal fistula, plus some fistulas are deliberately created by surgeons between an artery and a vein if someone needs haemodialysis for example. In this case, I want to talk about an enterocutaneous fistula which is my particular demon or angel depending on how you look at it!
So What Is An Enterocutaneous Fistula?
This can be explained by breaking down the words into their different parts:
‘Entero’ means bowel or gut.
‘Cutaneous’ means skin
‘Fistula’ is an abnormal connection between 2 surfaces.
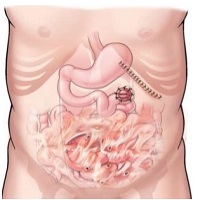
So an enterocutaneous fistula means an abnormal connection between the bowel and the skin.
Despite the fact they are viewed as a devastating complication 👿, they are actually saving your life 👼🏻. If the bowel contents resulting from a perforation collected inside you and did not come out via the fistula, you would develop sepsis and become seriously ill.
I try and remind myself of that every day but it’s not easy. I have never accepted my fistula and I struggle with it, not everyone’s coping mechanisms are the same. If a fistula is as a result of a life saving bowel surgery for example, then maybe it would be easier to accept, I don’t know. They cannot tell me why mine happened, I went in for a hysterectomy in pretty good health but ended up with a fistula. I did have a long history of chronic health problems, bowel disease for which I have an ileostomy plus severe endometriosis but the experts say these conditions have not caused the fistula. Attempt at repair two years later nearly killed me as I had respiratory failure. They cannot give me any medication as they cannot find any underlying disease yet it doesn’t heal. It’s not stable and causes frequent problems with infections and pain, often requiring a hospital visit.
So What Does This Mean For Me?
A fistula is a dreaded complication of surgery or illness – a complex medical and surgical problem that will need to be managed initially by a large number of healthcare professionals working as part of a multidisciplinary team. The team will focus on four main areas: sepsis, nutrition, anatomy and protection of skin.
The defects in the bowel produced by the fistula can result in bacteria leaking into the abdomen, causing a collection of pus. This is often referred to as ‘abdominal sepsis.’ If this is suspected, imaging (e.g. a CT scan) will be used to see where the collection is. The collection will need to be drained using a small tube and treated with antibiotics.
The main role of the bowel of course is to absorb nutrients from food and fluid. If there is a connection between the bowel and the skin, there is less time for the nutrients to be absorbed, and some nutrients will be lost through the fistula, usually into a bag placed over it. In addition, when the body is fighting infection it needs more nutrition than normal. Therefore, with less absorption and higher nutritional requirements, patients with fistulae can quickly become malnourished and lose weight. Electrolytes are the salts in the blood like sodium, potassium and magnesium. These are vital for many important functions, including regulating fluid balance and controlling our heart and muscle contractions. The problems with absorption can result in losing huge quantities of these salts from the body. This can result in dehydration and cramps which can lead to more serious complications. Whilst in hospital, the team may replace the salt and fluid using intravenous fluids or you may also be put on Trans Parental Nutrition (TPN) which means you will receive all your nutrition through a central line. This will ensure you get all the essential nutrients required amongst other things to facilitate healing, whilst resting your damaged bowel. TPN is called ‘liquid gold’ by some people as it is tailored to your individual needs depending on specialised blood tests. But like everything, there are massive down sides. I have been on it a few times for a few months at a time. Some people are never able to come off it.
Leakage from a fistula can be a distressing experience. The same enzymes in your gut that will digest a juicy steak will make contact with your skin and cause it to become excoriated, which means very red and sore with the skin breaking down just like that piece of meat. It is very painful and prone to infection which makes a bad situation worse. Therefore fistula care by the ward nursing staff, led by a specialist stoma nurse, is vital in preventing these problems. Medication may also be used to reduce the output and acidity from the fistula. You will see a stoma nurse when in hospital and a plan of care will be put in place for the ward nursing staff to follow. Once discharged you will have access to a stoma nurse if any problems arise. They will occasionally do home visits if necessary or you can go to the hospital.
The ongoing management of a fistula depends on so many factors. Each fistula is individual to that person and it’s very hard to generalise. Some people will have their fistulae repaired by undergoing more surgery. Unless faced with an emergency situation, there is usually a wait of at least 12 months before this can be attempted. Some people will have to continue to receive nutritional support at home (Home Parental Nutrition or HPN) through their central vein as the damage to the gut is too great and normal nourishment would mean essential nutrients would be lost resulting in malnourishment. In other words the food and waste would come out of the fistula before giving the bowel the chance to do its job – absorb all the nutrients and fluid from what we eat and drink. It depends of course on where in the bowel the fistula is. HPN tends to happen more with a fistula that is high up in the bowel, this usually means the fistula output is high (as much as several litres per day). If however the fistula is lower down and the output from the fistula is fairly low (under 200ml per day), then it’s usually possible to eat and drink normally, whilst wearing a stoma bag over the fistula. In my case I now wear two bags; one for the ileostomy which has served me so well for 33 years 👼🏻 and one for the fistula. My fistula is before my ileostomy so you’d think everything would come out of the fistula. Thankfully this isn’t the case. Most goes out through the ileostomy which is great news but some comes out of the fistula and whilst this connection remains it will never heal spontaneously.
If the cause of the fistula is found to be inflammatory bowel disease then sometimes medication can be given which will heal the gut and maybe the fistula. It is likely you will have to remain on these drugs for some time to control the underlying disease which may in turn keep the fistula closed.
Sometimes no definite cause can be found for the fistula and the patient may not be suitable for surgical repair. In these cases the patient will have to manage the fistula. This can prove to be very challenging, as it is likely the patient will need to wear a stoma bag over the fistula along with dealing with the daily problems a fistula can bring. As a fistula is quite often recessed into the skin ( unlike a stoma which has a ‘spout’), managing the bag can be tricky as leaks are often frequent but there are ways around this and your stoma nurses will be a valuable resource. I personally have found a wound bag to be most effective, it’s not pretty but it does the job, most of the time anyway.
A fistula is essentially a tube which our brilliant bodies make to keep us alive. Unfortunately infections in this tube and surrounding areas are common and may require periodic treatment with antibiotics and /or painkillers.
Fistulae are described as a surgical catastrophe. They are most certainly a very difficult complication which can be extremely challenging for the medical profession to deal with. However, the main challenges will have to be met by the patient – in my case, I have found it to be life changing. To go in for an operation in reasonable health and come out with a fistula is devastating. I had had a stoma bag for some 33 years previous to this and had managed it well, working full time and leading a normal life. I never even needed a stoma nurse. This however was so different and way more difficult and three years later it continues to be a big factor it my life. It’s not that stable and causes frequent sudden ill health meaning I cannot really have anything like the life I used to have. This is my new normal and I ( or I should say ‘we’ as it affects your nearest and dearest too ) are still learning to accept.
But we carry on and enjoy the good days. I am actually very lucky compared to some fistula patients but I am obviously very sad it happened and struggle with the ongoing consequences.
I hope this has given you some insight into what an enterocutaneous fistula actually is.








