In Brianna's case, Endometriosis didn’t just affect her uterus, read her story.

Blader & Bowel

In Brianna's case, Endometriosis didn’t just affect her uterus, read her story.

After enduring rounds of tests Melissa was finally diagnosed with endometriosis. Read her story.

What is Dementia, and how can you help someone manage continence issues? Read our...

According to Disability Rights UK, over 800,000 people will lose support for the extra...

Find out about third party research studies that you can get involved in -...

This recent guidance that has been published by NICE is for a new hormonal...

There are many products on the market that can help you feel more comfortable...

Join Health Panel to help contribute towards Ulcerative Colitis research and help future generations.

This month is Make May Purple for Stroke Awareness and we will be highlighting...

If you are a male and regularly self-catheterise, you can try LentisCath™ for free,...
Mike shares his experience and insights to help others who have their own struggles...

Nutrition and hydration week is a social movement which supports positive discussions between healthcare...

The Bladder and Bowel Community Facebook group has been supported since 2018, and now...

There are a number of alternative and complementary solutions to manage constipation and first...

More and more of us are turning vegan. In 2024 the number of Vegans...

The sober curious movement has been growing, and could provide a healthy balanced answer...

After festive indulgences, one of the ways that we can improve our health is...

Here at Bladder and Bowel Community, we’re already getting into the Christmas spirit. The...

If you suffer from a bladder or bowel issue or have any chronic health...

Staying safe and healthy during the Festive Season is important for many reasons, and...

We cover 4 common routes to care that you can try, if you’re struggling...

How bladder and bowel issues are affecting children at school Continence conditions are the...

Do you ever get frustrated by the ‘admin’ involved with healthcare? Home delivery brings...

After having her gallbladder removed Helen experienced severe bowel issues that had a hugely...

Are you struggling to manage bladder leaks? Jude, a community focussed bladder care company,...

At Bladder & bowel Community we’ve been working in the background to bring you...

If you’re among the millions of people who struggle with bladder issues, you know...

When living with a chronic illness it can be difficult to start and maintain...

Kate Rock is a certified Yoga teacher who has undergone additional, specialist training in...

Have you ever wondered how those super-energetic people do it? Those bouncy people, who...

Katie Highton, aged 23 from the Scottish Borders has lived with bladder dysfunction for...

Zoe McKenzie is a Physiotherapist, Personal Trainer and Pilates Instructor who lives with several...

In this fast-paced world that we live in, taking care of our bodies often...

We're championing kidney health. Do you really know about the importance of your kidneys...

In this blog post, we'll explore practical tips to ensure you are well equipped...

Kidney health is one of those aspects of health that often gets overlooked. How...

Winter is a time to slow down, focus on comfort and spend time nourishing...


It’s easy to feel disconnected during the winter months. When the weather is bad...

Good food is so much more than just the sum of its nutrients. It...

Susan Jardine, from Preston, Lancashire is a carer for a gentleman called James, who...

For those with a bladder or bowel condition, the thought of having to travel...

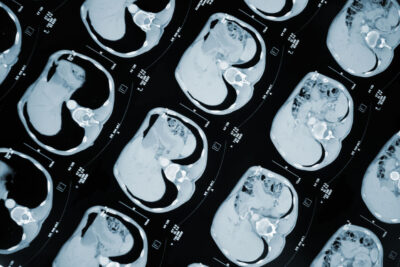
After years of escalating bowel issues, Mark was eventually diagnosed with Crohn’s Disease in...

David McVey, 58 from Glasgow noticed that he was having trouble going to the...

Helen Brook, 36 from West Yorkshire had struggled with bowel symptoms since her teens...

A new 'Turbo' radiotherapy treatment for men diagnosed with prostate cancer could dramatically improve...

When Rocco Mann, 20 from Banbury in Oxfordshire was first diagnosed with Crohn’s Disease,...

Jordan Bew, 36 from Cornwall spent nearly 2 years suffering from crippling, painful bladder...

World Continence Week ran from the 19th to the 23rd June and is an...

Deciding to get help with anything, let alone, medical concerns can be a challenge...
Marcus, from Kent was diagnosed with bladder incontinence around four years ago, however he...

Whether you’ve been living with bladder weakness (incontinence) for years or if it’s...

We were heartened to hear Gemma Collins’ own account of her ‘accident’ whilst playing...

March is Ovarian Cancer Awareness Month and this month we want to help shout...

Last year, the Bladder and Bowel Community launched their own toilet scheme where high...

'Invincible Claire' was diagnosed with premature ovarian insufficiency and thyroid disease, after trying to...

Anna Cooper, 29 was diagnosed with endometriosis at the age of 17. She spent...

When Sheree Hargreaves aged 15 realised that all her friends had started their periods,...

Coeliac disease, also known as celiac disease, is a serious autoimmune condition that can...

Over 1 in 10 people in the UK are thought to have Irritable Bowel...

With many of us starting to become affected by the cost of living crisis,...

Christmas is a wonderful time where we can celebrate with family and friends. It...

Amy Davidson tells her incredible story of how she grew up with Hirschsprung's Disease...

There are many practical ways to keep yourself safe, and it’s not all about...

In recent months we’ve been working to raise awareness of the issues faced by...

Laura MacKenzie, 45 from Wemyss Bay was diagnosed with a rare and aggressive type...
We’re supporting Marks & Spencer with some vital market research to help them understand...

Thank you for confirming your preferences, we will do everything we can to remove...

Irritable Bowel Syndrome (IBS) is a function disorder of the gut and is thought...

We’ve developed a new scheme to help educate staff who work in the retail...

Community member, Anna Somerville-Large has kindly shared her story with us about living with...

The cost of living crisis has pushed up food prices and has meant that...

Google has announced that Google Pay will be reverting back to Google Wallet and...

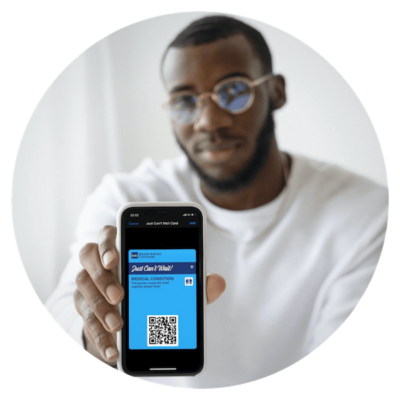
Introducing the national Just Can’t Wait Toilet Scheme for participating businesses and organisations to...

Elaina Cutting joined the Bladder and Bowel Community Support Facebook group after experiencing bowel...

The Bladder and Bowel Community has partnered up with some great companies to be...

Flaxseed has been well researched in recent years and has gained the reputation as...

The Hidden Disabilities Sunflower is here to help overcome some of the barriers faced...

Mags tells us how a chance listening to Deborah James' (aka Bowelbabe) podcast ‘You,...

Many people living with irritable bowel syndrome are vitamin D deficient, according to a...

Travelling with bladder and bowel conditions can be a stressful process, and many will...

Lucinda Barton suffered with what she was told was Irritable Bowel Syndrome for over...

A recent worldwide study has revealed that there is a close link between having...

Public Toilets are never going to be a glamorous topic. Nevertheless, we all need...

The first RADAR locks were fitted in 1981 to help keep accessible toilets free...

What is endometriosis, and what are the symptoms caused? We share three community stories...

During February we organised a catheter awareness week on our social media channels to...

One year after going digital, the Just Can’t Wait Card is relied on by...

Abbie Stapleton, 25 from St Neots tells Bladder and Bowel Community how endometriosis and...

Zoe, 24 from Oxfordshire/Northamptonshire border tells Bladder and Bowel Community how one day...

Natalie, 39 from London was diagnosed with Stage 4 bowel cancer at the age...

In this video for Catheter Week, Estelle Stevens, 37 from Devon talks to the...

Welcome to Catheter Week where we’ll be discussing all things catheter, to offer support...

Today’s spotlight is on Fowler’s Syndrome, a little known bladder disorder that affects women...

The Just Can't Wait Card petition has reached 5k signatures. We caught up with...

Coeliac Disease is a little known condition where the body’s immune system attacks the...

This campaign encourages us to check for any unusual changes in our ‘Bathroom Health'...

We asked our community what they will be doing differently this year, and here’s...

Community member Tara Dolman has raised a petition to get the Just Can’t Wait...

This Urology Awareness Month, we have worked with the ME Association to highlight how...

The gut has long been called ‘the second brain’ so it stands to reason...

Dionne, 23 from Scotland talks to Bladder and Bowel Community about how the perception...

When Deborah decided to help boost a friend’s confidence after undergoing stoma surgery, she...

We're highlighting the importance of early detection by knowing the symptoms of bladder cancer. David...

Saffronne Epaminondas has lived with IBS for over 32 years and was diagnosed at...

For mental health awareness week, Community Manager Gemma Savory describes ways to help you...

Fashion designer, Victoria Jenkins tells us about how her own health issues and how...

Having a child with a bladder or bowel issue can be scary and frustrating...

Three years ago, Niki Wells shared her story with the Bladder and Bowel Community...

Around 14 million people in the UK live with a bladder condition and over...

The original toilet card from the Bladder and Bowel Community is now available on...

The Just Can’t Wait Card is now available as a Digital Pass on Apple...

For such a common condition as incontinence, it’s important to understand exactly what help...

Provided in its present form since 2017, we are proud to now have over...

Here at Bladder and Bowel Community, we’ve been looking to the future to see...

We are working hard to ensure a continued high level of service for you...

In a recent customer satisfaction survey, 96% of our customers told us they would...

Stoma bloggers have done such a lot to reduce barriers around some key topics....

We highlighted #stomaweek here at Bladder & Bowel Community, with a focus on stoma...

As part of #stomaweek, Keith Thomas, 59 from Llanelli shares his story on how...

This week we’re talking ‘All Things Stoma’. We’re always looking for ways in...

It’s not uncommon to struggle with diet for IBS - knowing what your triggers...

When we talk about having a bladder or bowel condition, we mostly talk about...

With lockdown restrictions lifting further still, and with the recent announcement that shielding for...

With the emergency of COVID-19 this year, we have all found ourselves in this...

Jan Ross underwent stoma surgery in February this year just before lockdown, after being...

We talked to Physiotherapist and Founder of Actively Autoimmune, Zoe McKenzie to get her...

Updated 10th July 2020 With so many shops, cafes and pubs reopening their doors...

Director Joanne Umbers represents the Community in the discussion around public toilets As...

At-home, finger-prick blood tests mean that you can test various health indicators yourself. Whether...

You can order a free sample of MoliCare® pants for Men or Women. As...

Welcome to our dedicate a space where we talk about all matters relating to...

At Bladder and Bowel Community, we don’t want anyone to struggle or feel lost...

Bladder & Bowel Community member, Anne Fairhurst shares her experiences of living with Megacolon...

Due to the recent raised concern around the Coronavirus outbreak we feel it is...

Introducing Hannah, who will be contributing as a regular guest blogger for the Bladder...

Crohn’s and Colitis are invisible illnesses that mainly affects the digestive system but can...

Bowel Cancer UK has launched its annual Decembeard campaign aimed at raising awareness and...

Are you affected by diverticulitis? Would you be interested in helping to shape the...

Sore skin. Bag leakages. These four words are a common source of anxiety for...

We are pleased to announce a new partnership with StrategiQ, an award-winning marketing agency...

This week is Diabetes Week and Diabetes UK are working to raise awareness of...

If we have a physical illness most of us wouldn’t think twice about contacting...

Elvie Trainer is a small and smart pelvic floor training tool that helps you...

How much do you know about your kidneys? These two fist-sized beans do more...

Tara has agreed to share her story with the Bladder and Bowel Community. Tara...

It has been just over four years since you came into my life, but...

Jeff Finnie, aged 51, from Swindon is running 20 half marathons in 20 months...

This week is Crohn’s and Colitis Awareness week. Crohn’s Disease and Ulcerative Colitis are...

Student Film makers aim to raise awareness of invisible illnesses like inflammatory bowel disease...

Urinary incontinence is the inability to control your bladder, causing unwanted and involuntary leakage...

We are proud to provide an essential support service in the form of the...

We were interested to see that included in today’s Budget 2018 news was the...

Mark has bravely agreed to share his story of living with an overactive bladder....

Yesterday marked World Menopause Day and an opportunity to discuss a change in life...

On World Mental Health Day, Bladder and Bowel Community Manager, Gemma Savory talks about...

Fistulas are usually caused by injury or surgery, they may also form after an...

Niki Wells is 33 years old and lives in London with her partner Dany,...

We are so pleased to announce that we have been chosen as a finalist...

After months of suffering, Muneeb was diagnosed with Crohn’s Disease in October 2016, aged...

If you are currently receiving chemotherapy treatment for metastatic colorectal cancer with mets to...

How many of us when we are younger try to map our lives out?...

Today the NHS turns 70 years old and Bladder and Bowel's Community Marketing...
Time 2 Talk Ostomy Support Group is a new group for those who want...

Low testosterone, also called andropause, Low T, or testosterone deficiency is the male version...

By Gemma Harenburg: So the story really begins since I came home. The background...

Stress Urinary Incontinence (SUI) is a very common condition, affecting an estimated 30% of...

Few conditions can claim to be the subject of quite as many misconceptions as...
Being diagnosed with a bowel condition is a life-changing experience, and most are simply...

Georgia is 24 years old and has a very rare chronic bowel motility disease....

This week is MS Awareness Week (23 - 29 April), Multiple Sclerosis affects thousands...

Cara found herself staring bowel cancer in the face at only 32 years old....

The Kegel exercises are important for women to maintain healthy and strong pelvic floor...

This week is Autism Awareness Week and we have been speaking to Louise Fields...

Poor nutrition and hydration can sometimes make bladder and bowel symptoms worse, this article...

Today, many people lead such busy lifestyles that health all-too-often gets pushed to the...

Urinary bladder function is an important to your health. Find out how to empty...

Travelling with bladder and bowel conditions can be a stressful process, and many will...

Urinary incontinence can be painful, embarrassing, and even debilitating. Whether it is yourself, a...

Have you recently been diagnosed with incontinence? Maybe you’ve been experiencing symptoms and you’re...
My name is Gemma and I have cancer. In fact, I have Stage 4...

We are committed to publishing the latest news and information from the community and...

On 28th February 2018, Plymouth Hospitals NHS Trust will be running a Bladder And...

Laura is a busy new mum, a nurse and at the young age of...

As many ostomates know, a ‘usual’ stoma care routine can involve many pouch changes...

Natalie Toper, Cancer Counsellor and bowel cancer survivor is campaigning to get stoma signs...

The Royal Society of Medicine will be holding a seminar this March which will...

Cancer charities Bowel Cancer UK and Beating Bowel Cancer have today announced that they...

Harriet Foulkes-Arnold, 34 from Shrivenham, suffered from leaks after having her first baby and...

Calling all men! Ditch the razor this month, create a little extra winter warmth...
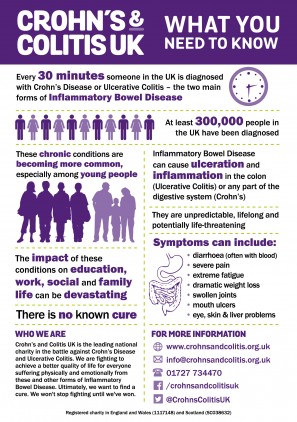
Crohn’s and Colitis Awareness Week takes place each year between the 1st and 7th...
We’re always grateful to our community for sharing their stories and letting others know...
Elaine Miller is a successful physiotherapist that has worked in the glamorous field of...

It’s a natural part of our life and we all do it (in one...

If you have Inflammatory Bowel Disease or an ostomy then you probably know who...
We’re always grateful to our community for sharing their stories and letting others know...

We spoke to BBC Radio Essex this week to give our opinions about a...

Meet Lauren; she suffers with a bowel condition called Irritable Bowel Syndrome, which has...

Living with a bladder condition such as Overactive Bladder can be both physically and...

In January 2016, Fi Munro was diagnosed with Stage 4 Ovarian Cancer. At the...

What does ‘welcome’ really mean? We often see the outside of Buckingham Palace on...
Lauraine has IBD, which has resulted in an ileostomy and she also suffers from...

This week we’ve all been inundated with those photos of cute smiling kids in...

In support of our work in campaigning for publicly available toilets for people suffering...

Struggling with Bladder Weakness? Tired of just managing the symptoms?

Share your story with the Bladder and Bowel Community and help us to raise...

At Bladder & Bowel we’re constantly working with our partners to bring you the...

Leading bowel charity, Bowel and Cancer Research have created a new identity to cement...

At Bladder & Bowel we love to talk to the amazing people in our...

Shared toilet scheme for Gravesend following further public toilet closures Recent local news reports...

Want to know what foods irritate the bladder, or calm the bladder lining? We...

The NHS Liverpool Clinical Commissioning Group has recently announced that they will be holding...

This week the Colostomy Association launched the theme for these year’s Colostomy Day. Every...

The Bladder and Bowel Community team will be taking to their cycles again on...

There are many stages of life which pose new challenges and it’s easy to...

Published on 20/6/17 Being a family carer is a demanding role and one which...

It is usual for anyone who is about to undergo an operation to have...

AD This article contains links Published on 20/6/17 The impact of urinary incontinence on people’s...

Published on 20/6/17 Did you know that you can visit a continence clinic without...

Published on 20/6/17 Incontinence impacts more than 200 million people worldwide and between three...

Designed by chartered physiotherapists specialising in Pelvic Health working in the NHS, Squeezy is...

INNOVO® is working in association with the World Federation of Incontinent Patients (WFIP) for...

“Desperate for the loo? They’re closed now but they’ll be open for the summer...

Post Prostate Cancer surgery? Suffering with leaks? A revolutionary, new incontinence treatment has got...

AD This article contains links Dr. Ruth Maher is one of the original four...

The Bladder and Bowel Foundation has been serving the Bladder and Bowel Community since...

Morrisons install accessible toilet signs in 492 stores. The Bladder and Bowel Community is...

We are delighted to announce that Blake Beckford has been shortlisted for Business Person...

Amongst other things, April marks IBS Awareness Month. So we thought it would be...

Millions of people in England experience problems with continence but many are not getting...

Scientists claim method is potentially more accurate than PSA and could minimize predicament of...

A newly-launched Cancer Research UK study could be the first step towards exercise training...

Benjamin King, star of Disney Channel's hit TV series Liv and Maddie, helps others,...

New evidence published highlights benefits and harms of using artificial mesh when compared with...

A report into the financial and emotional costs of constipation has been launched on...

On Tuesday 16 February, Improving Quality in Physiological Services (IQIPS) hosted its very first...

Up to half of samples of urinary tract infections in children are resistant to...

Researchers at the University of Sheffield have developed a novel implantable material which could...

NICE has issued final guidance recommending abiraterone (marketed as Zytiga by Janssen) for some...

New early warning system to prevent life-threatening urinary infections in catheter users. A new...

Ahead of Continence Awareness Week to be staged in June, the Chief Nurse for...

On July 2nd this year, Mike Quinn (Miromedia) is riding with 14 like minded...

Elaine Miller is a physiotherapist based in Edinburgh. She wrote a comedy show about...

Dr. Adrian Wagg, from the University of Alberta, is conducting a survey exploring women’s sources of information, knowledge...

The purpose of the NHS England self-assessment framework for continence is to:

Bedwetting, or nocturnal enuresis, causes distress in children and young adults, as well as...

Thousands more people would take part in bowel cancer screening if the kit included...

Dynamic pelvic floor magnetic resonance imaging (MRI) is a non-invasive test that uses a...

Current therapies for children with Crohn's disease don't fully restore healthy bacteria and fungi...

NICE has developed medical technology guidance on the UroLift system.

A new understanding of inflammatory bowel diseases has been prompted by the analysis of...

One of the most common, but rarely discussed issues that female athletes face is...

Training in meditation and other mindfulness-based techniques brings lasting improvements in mental health and...

September 16th 2015 marked the momentous achievement of 100 years of the WI. Much...

NHS England has today published new guidance to help improve the care and experience of...

The Royal College of Obstetricians and Gynaecologists (RCOG) has recently published a Recovering Well...

Clinicians in Southampton are set to lead a pioneering UK study into the use...

Dr Martin McShane's Blog:I was at a roundtable on how health and care services...

New research could lead to new treatments to prevent blockages and urinary tract infections...

Report by Professor Dame Sally Davies targets obesity and ovarian cancer and encourages women...

After menopause, more than half of women may have vulvovaginal symptoms that have a...

UK patients with ulcerative colitis gain access to a range of biologic therapies on...

This quality standard covers the management of urinary incontinence in women aged 18 years...

The Telegraph has reported that Health Secretary Jeremy Hunt will call for hospital managers...

In July NICE published new guidelines on safe staffing for nursing in acute hospitals.

Shadow Health Secretary Andy Burnham has given a speech on health and social care...

Children who start toilet training before age 2 have a three times higher risk...

Men with a specific pattern of baldness at age 45 have a 40% increased...

Prostate cancer is the second most common cancer in men around the world, but...

Scientists have given us many reasons not to smoke, but now, researchers from the...

You've probably heard your GP mention Continence Advisors and Continence Physiotherapists before, but do...

If you would like to view a helpful video about how pelvic floor muscle...

NICE have published a guideline on bladder cancer. This guideline offers evidence-based advice on...

The results of a clinical study were recently published, looking specifically at the use...

Astellas Pharma Europe Ltd. has announced new data from the Phase 2 TERRAIN trial...

According to study author Prof. James Morris of the Vancouver Cancer Centre at the...

Older women with urinary tract infections who are taking the commonly prescribed antibiotic nitrofurantoin...

Trillions of microorganisms colonize our gut and together form the intestinal flora that coats...

The National Institute for Health and Care Excellence (NICE) has published final Technology Appraisal...

Two national charities are launching a social media campaign, 'Love your Gusset!', to empower...

Many women have to get up more than once a night because of a...

Some previous studies have linked the diabetes medication pioglitazone to bladder cancer.

Researchers at Georgetown Lombardi Comprehensive Cancer Centre have completed a critical step in the...

Incontinence is treatable. It is therefore essential that assessment of incontinence is sought...

Labour MP Rosie Cooper has tabled two written questions on continence care and UTI...

Researchers found that capsaicin - the ingredient that gives chili peppers their heat -...

UCLA researchers interviewed people with diverticulitis and confirmed that many suffer psychological and physical...

Interstitial cystitis/bladder pain syndrome (IC/BPS) is a disorder with symptoms of mild to severe bladder pain and an...

Researchers at Queen's University have made a significant breakthrough that may benefit patients with...

Colorectal cancer has been linked to carbohydrate-rich western diets, but the underlying mechanisms have...

The Care Quality Commission (CQC) has published expert analysis on the way people experience...

Dr Martin McShane, NHS England's Director for Patients with Long Term Conditions, explains why...

A new study, published in the UEG Journal reveals that 10% of IBD patients...